X-linked agammaglobulinemia (X-LA) is caused by mutations in the
BTK gene that encodes Bruton's tyrosine kinase, resulting in the arrest of B-cell development (
Bruton 1952;
Tsukada et al. 1993;
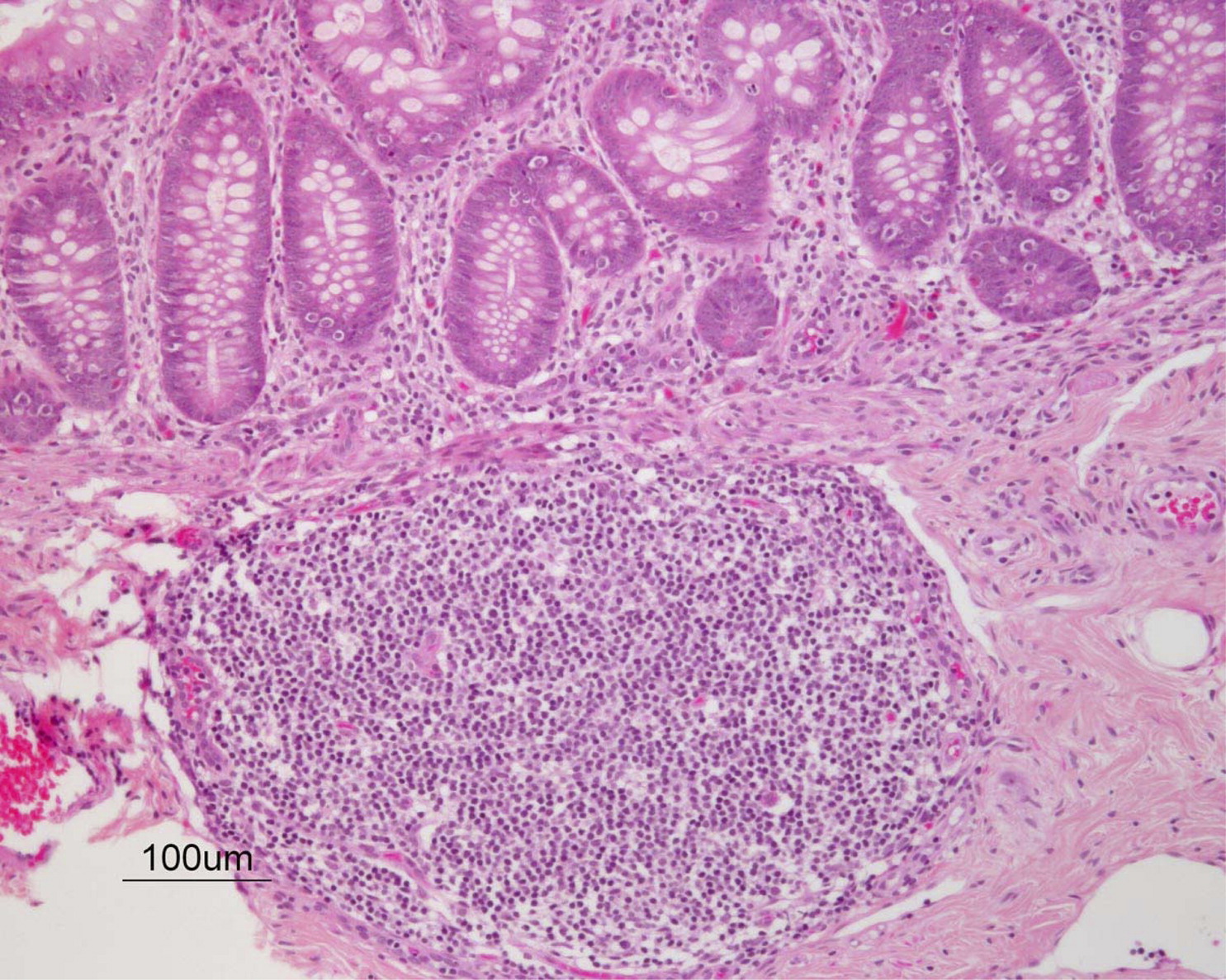
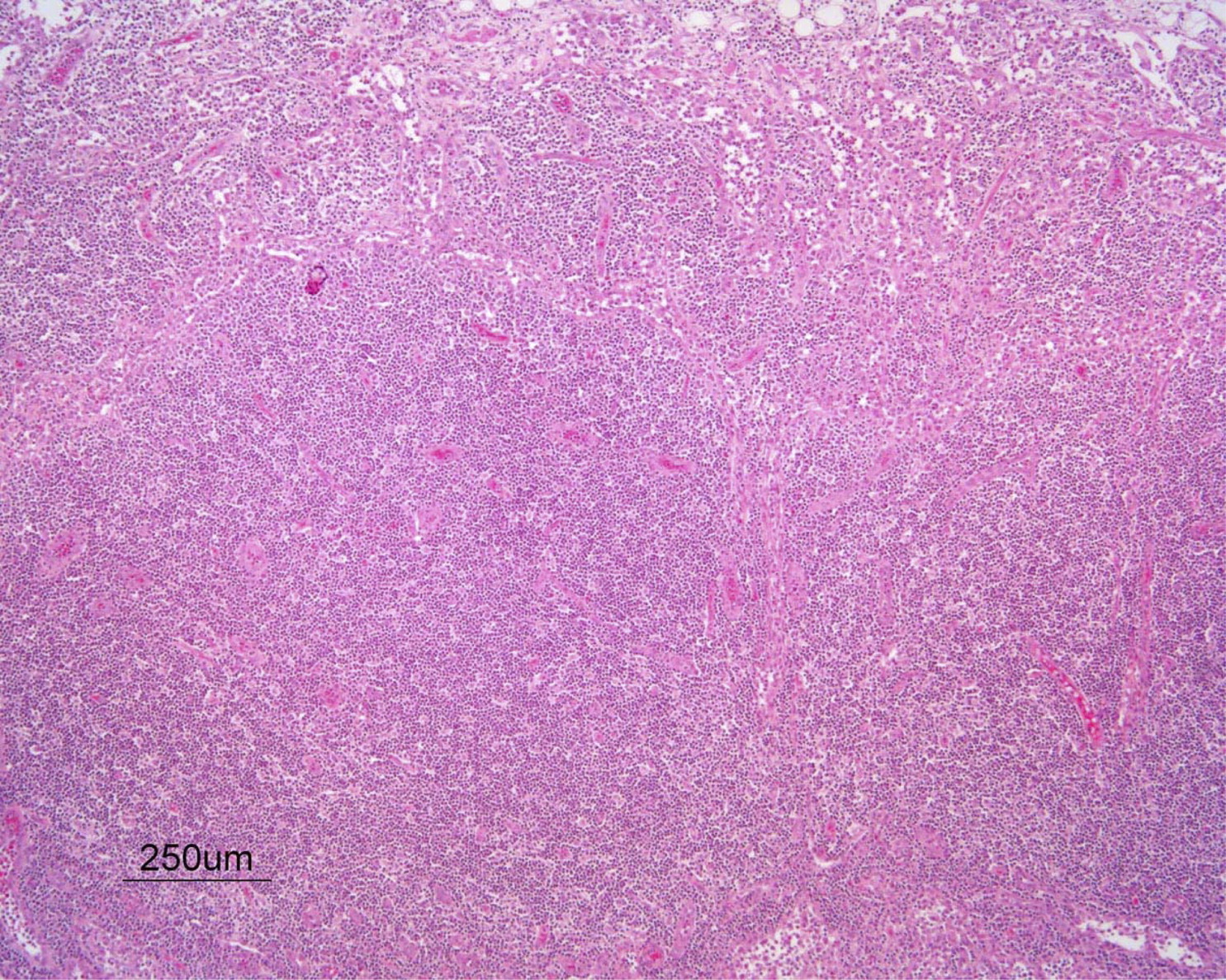
Vetrie et al. 1993). Characteristically, these patients have no visible tonsils, no palpable lymph nodes, no detectable circulating B-cells dysplatic lymph nodes (
Figures 1 and
2), and extremely low-to-absent serum levels of immunoglobins G, M, and A (IgG, IgM, and IgA). As a consequence patients may suffer repeated and sometimes fatal infections with encapsulated bacteria and enterovriuses unless treatment with IgG replacement is administrated.
Unfortunately, unless a family history exists, this condition may not be suspected or detected in a timely fashion for several reasons:
1.
This a rare condition and is usually not suspected by primary care providers.
2.
Symptoms most frequently include upper respiratory infections and otitis media, which are common in the “healthy” pediatric population.
3.
Maternal–fetal transfer of IgG provides protection from microbial infections during the first few months of life.
The following case, together with other cases as presented by Nahum et al. on page
75, highlight the need for promoting tools for the early diagnosis of this condition.
A male, 2 years and 4 months of age, born to nonconsanguineous parents of Polish descent, suffered from repeated upper respiratory tract infection and otitis media from the age of 6 months. Myringotomy tubes inserted at 1.5 years of age reduced morbidity dramatically. On examination he had palpable lymph nodes in the cervical area and his growth and development were appropriate for his age. At 2 years of age he was admitted to hospital for fever, coryza, and cough lasting several days. Upon examination, he was found to have lymphadenopathy in the cervical area. A throat swab was positive for Group A streptococcus and he responded well to antibiotic therapy. Three months later he was examined in an emergency room for a 3-day course of fever, coryza, and vomiting. He was sent home with a possible diagnosis of a viral infection, only to return 24 hours later with persisting fever, red eyes, diarrhea, hypotension, and tachycardia. A CT scan revealed cervical adenopathy on the right and left neck mass abscesses (
Figures 3–
5). Petchiae were noted on the arms, face, and chest. Immune evaluation revealed normal numbers of circulating CD3
+ T cells at 2800 cell/µL, of which 2100 were positive for CD4 and 820 were positive for CD8. CD19
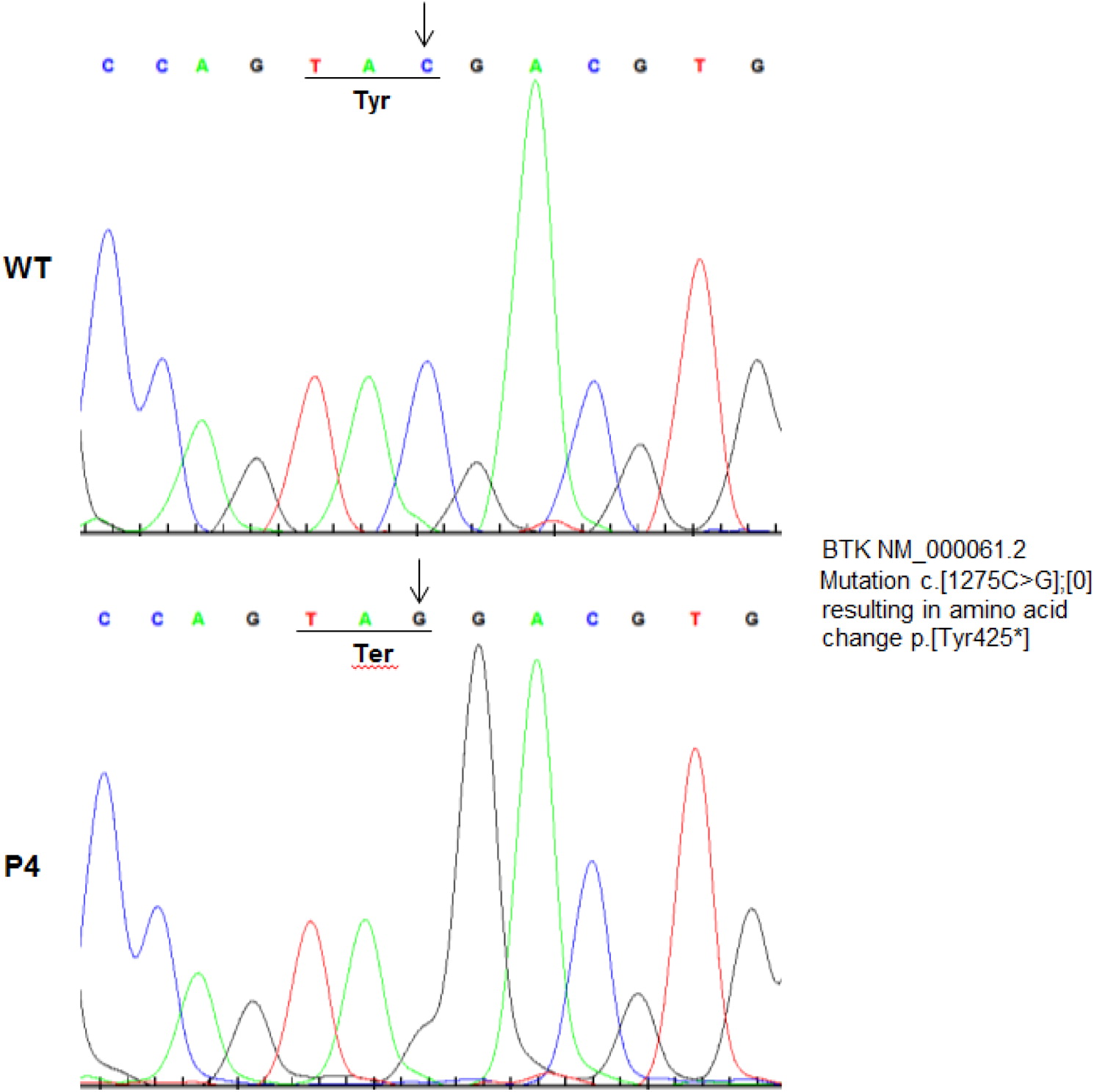
+ cells were not detected. The patient's IgG, IgM, and IgA were absent. Sanger sequencing showed a C to G transition at position 1275, creating a premature stop codon at amino acid position 425 in the tyrosine kinase domain (
Figure 6). He rapidly deteriorated, developing seizures and respiratory failure. He was admitted to ICU with the diagnosis of septic shock and coagulopathy. Blood count showed neutropenia and lymphopenia, and blood cultures were positive for Group A streptococcus. Despite intensive management, the patient's condition rapidly deteriorated and he died of multi-organ failure 9 days after admission.
Autopsy showed lymph nodes in the neck, axilae, and mesenterium. Histology revealed absent germinal centers and very few CD20+ B cells but a normal number of CD3+ cells. The spleen had no white pulp and B cells were absent. Gut-associated lymphoid tissue was hypoplastic with no germinal centers or B cells.
Kappa-deleting recombination excision circles (KRECs) are circular DNA segments generated in B-cell precursors during maturation in the bone marrow. These DNA elements persist in the cells but cannot replicate and, therefore, get diluted with every cell division. Their quantification thus, can serve as markers of B cells lymphopoisis. Recently, the development of reliable real-time quantitative PCR methods has allowed for early screening and detection of conditions that interfere with normal V(D)J recombination such as agammaglobulinemia and several types of severe combined immunodeficiency.
It is alarming that even at this age of modern health care, including intensive care and pharmacologic advancements, X-LA remains a potentially fatal inherited disease. Together with ample evidence for a heavy burden of morbidity in these patients, early diagnosis prior to development of infection is of paramount importance. With the recent development of reproducible methodology for detecting KREC's in Guthry blood spots, this should be added to newborn screening programs as a lifesaving procedure.